Our Extraordinary Pharmacy Program Results in Extraordinary Outcomes for You
Discover the Enlyte Difference
For many Pharmacy Benefit Managers (PBMs) group health is their focus, and workers’ compensation and auto casualty are an afterthought accounting for around 1% of their business.
100% of our focus, investment, and expertise is directed at supporting our work comp and auto casualty customers. Our PBM solution features extensive clinical oversight, innovative and unique technology, and seamless integration with bill review, utilization review, and case management.
Enlyte Delivers
1. Intersecting bill review and pharmacy solutions ensures clinical oversight of out-of-network pharmacy transactions from third-party billers, physician dispensers, and co-mingled medication bills for increased savings.
2. Greater visibility and clinical management leads to fewer high-cost prescriptions being filled, ensuring you don’t pay for inflated drugs when more cost-effective alternatives are available.
3. When adjusters and nurses have insight into high-risk and high cost claims they can act immediately and mitigate increasing claim costs.
4. Our dedicated team of pharmacists, client service managers, and regulatory experts support our pharmacy program with tools, reporting, and guidance to identify price opportunists.
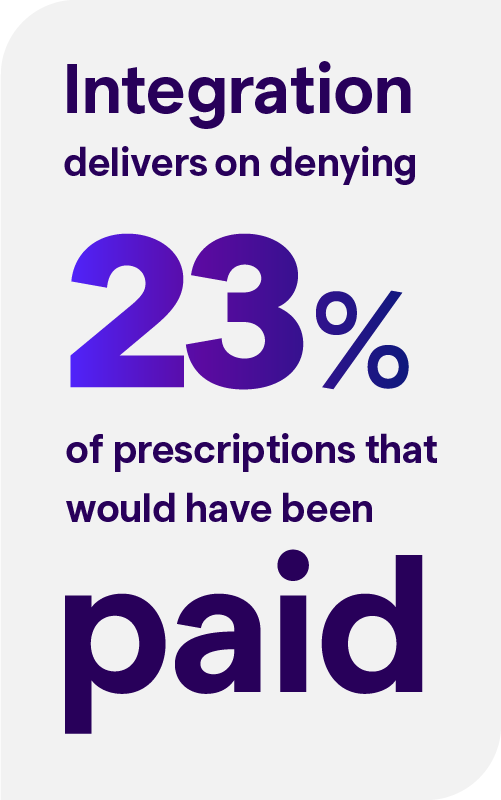
Our Proven Value
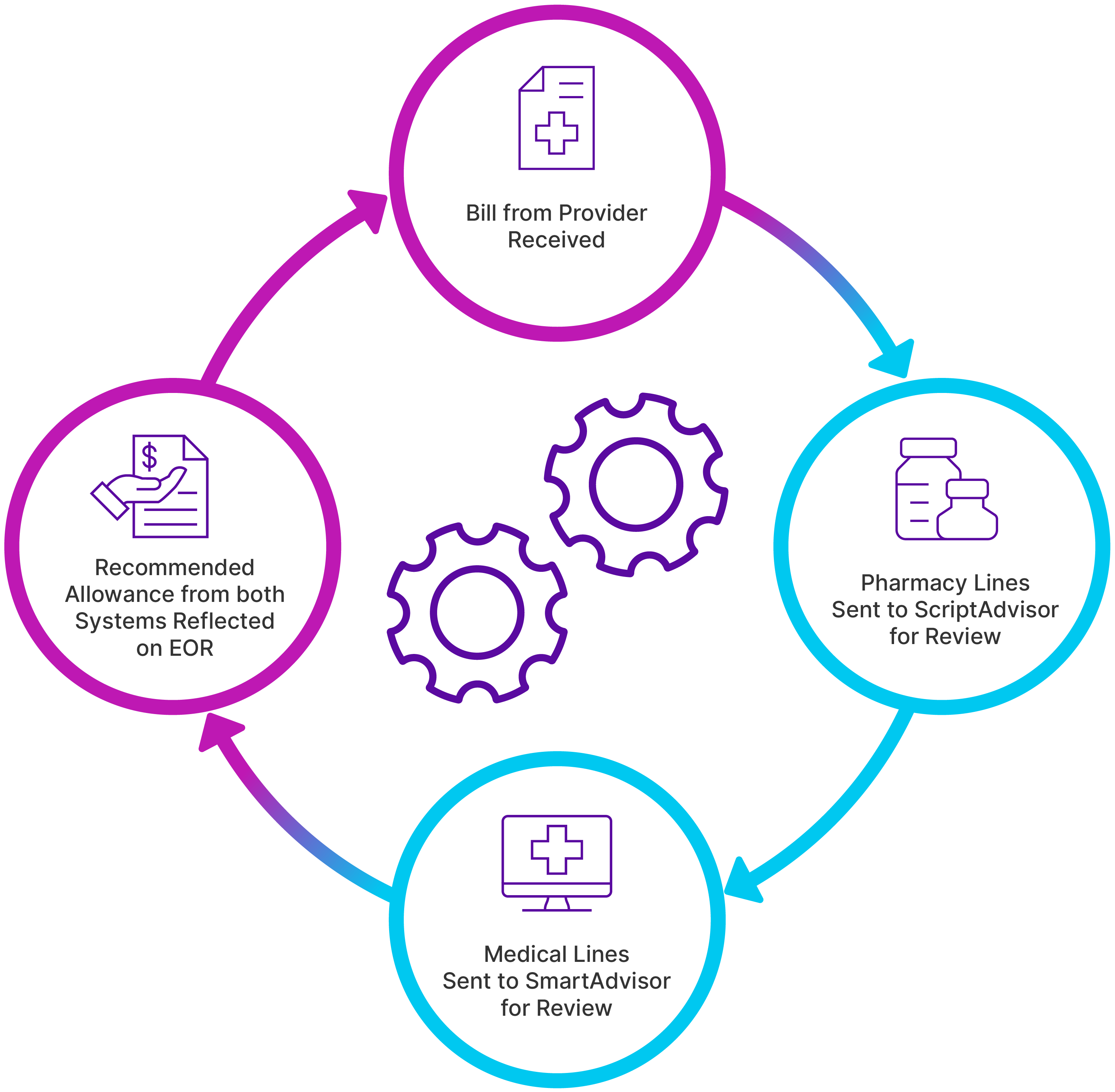
Bill Review + Pharmacy Benefit Management
Keeping up with endless industry changes is no easy task. Enlyte’s leaders are constantly interacting with clients, like you, to ensure we know exactly what’s keeping you up at night and working to create solutions that impact your bottom line. Listen as our experts discuss their predictions for 2024 and beyond. Then let us help you align a strategy to tackle them head on.
By integrating bill review and ScriptAdvisor pharmacy solutions you can achieve 100% visibility into your pharmacy spend.
Efficiencies
- Reduced decision-making time using a single location to manage all bill review and pharmacy decisions for adjusters/case managers
Outcomes
- Improved PBM in-network penetration through network application and reindexing
- Increased clinical savings with embedded pharmacy workflow for commingled bills
Savings
- Applying clinical edits and network pricing to your out-of-network spend can improve network penetration by up to 13%, saving 54% off fee schedule
- Life-of-claim risk identification leveraging medical pharmacy data
Visit Our Full Solutions Pages to Learn More
“Having the bill review program and the ScriptAdvisor program integrated gives enormous ease of use.”
—VP of Claim Operations, Regional Carrier