Applications of Predictive Analytics in Workers’ Compensation
As technology use continues to rise in almost every facet of today’s society, the mark it has left on the property and casualty industry, specifically within workers’ compensation, isn’t surprising. From artificial intelligence to machine learning and telemedicine, there’s no denying that technology is here to stay—and rightly so. One specific technology that’s becoming more popular in this particular space is predictive analytics. PropertyCasualty360 states that predictive analytics is “the secret weapon for P&C insurance.” Why? Let’s learn a little bit about how predictive analytics is shaping the industry today.
2021 Mitchell Survey Supports Predictive Analytics’ Increased Impact
In February 2021, Mitchell surveyed roughly 100 workers’ compensation leaders to evaluate the technologies that played the biggest roles at their company, understand how those technologies affected their business, learn more about the industry trends they witnessed in the market and hear about the major challenges each organization faced. The list of technology adoption ranged widely from telemedicine to electronic billing and payments to mobile capabilities to predictive analytics and more.
Download the full report now for a deeper dive into our 2021 survey results.
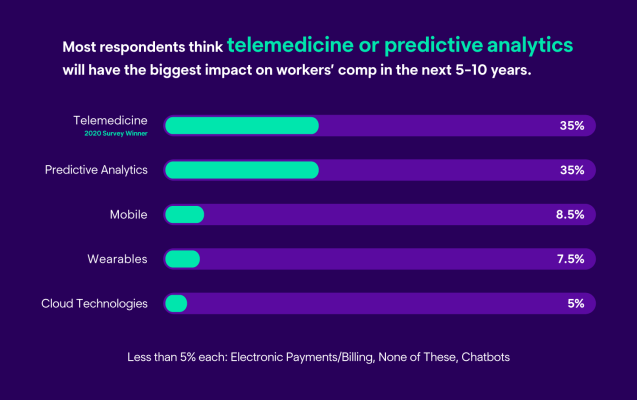
In this year’s survey, we asked respondents which technologies they think will have the biggest impact on workers’ compensation in the next five to 10 years. Predictive analytics and telemedicine shared first place at 35% each, whereas in our 2020 survey, telemedicine led with 32%, artificial intelligence ranked second at 30% and predictive analytics represented in third place. Our survey results show that predictive analytics is making significant headway in the industry, especially considering the high percentage of votes predictive analytics received in 2021, compared to our 2020 survey.
Predictive Analytics
Predictive analytics is not a “one-and-done” technology; it has many applications that span across the entire claims process. From enabling alerts and actions about claims that are approaching an unanticipated direction to redirecting claims to the right people at the right time, it’s no surprise that predictive analytics seems to be sparking interest within the workers’ comp industry. To verify the rise in popularity, we asked respondents in our 2021 survey what technology they believed would be the most influential application of predictive analytics. The selections included: claim triage, severity or reserving, intelligent decisioning and adjuster guidance, claim automation, clinical referrals and SIU/provider behavior. Claim triage, severity and reserving and intelligent decisioning (35%) and adjuster guidance (23.5%) came out on top.
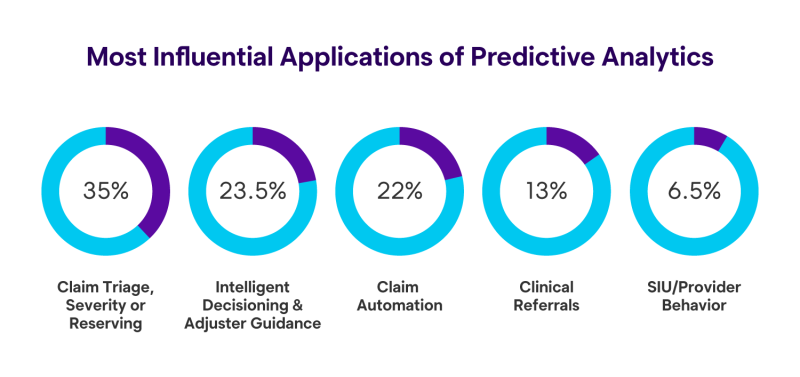
The results convey that claim triage, severity or reserving and improving intelligent decisioning and providing adjuster guidance are the main areas the industry will focus on applying predictive analytics to next. Organizations use characteristics of the claim to adjust workflow, assist in decision-making, categorize claims by severity and guide claims staff, all of which are essential, in our eyes, to claims handling. With that in mind, let’s take a look at how predictive analytics is impacting these two areas.
Benefits of Using Predictive Analytics to Improve Claim Triage, Severity and Reserving
The use of predictive analytics can help organizations improve claim triage, severity and reserving. Correct claim triage early on is important to successful claim outcomes—to achieve this, claims organizations should have consistent practices within their adjuster workforce to direct claims to the right individuals in a timely manner for maximum success. Using predictive analytics to facilitate early triage can help companies avoid scenarios where one person spends time reviewing a claim, only to find out that it requires assistance elsewhere. Using predictive analytics can also allow claims organizations to appropriately route claims for straight-through processing, for example, by automatically routing simple claims for straight-through-processing and sending more complex claims to highly experienced or specialized adjusters.
Using predictive analytics early on may also help to predict claim severity and recovery timelines, helping set the claim down the right path from the start and flag the claim if it starts to go off course. Using predictive analytics for early identification of claim severity enables claims organizations to identify claims that might benefit from more of a human touch. If the need for case management can be identified early, organizations can ensure that an injured employee has an advocate – someone who can help clear the way for speedy recovery. Identifying the need for case management may happen early on in the claim workflow or could happen later as the claim progresses. Either way, technology can help ensure a better outcome, one that helps the injured employee return to full health sooner.
Another way predictive analytics helps with the claims triage process is by ensuring that the claimant is assigned one claims professional to engage with from the start, improving consistency and simplifying the communication process. When an injured employee speaks with one claims professional throughout the entire process, instead of bouncing back and forth from one person to another to discuss matters about the claim, it not only creates a consistent experience for the injured employee, but can also help the claims organization manage costs, provide better care and facilitate appropriate intervention earlier on in the process, ultimately creating a more positive end-to-end experience.
Finally, predictive analytics can also be used at the start of the claims process to help companies better understand what actually caused the injury, which is useful if the claim is litigated, since this technology can help provide scientifically-supported talking points for attorney-represented claims, such as flagging potential inflated or exaggerated claims.
Here is a recap of the benefits that using predictive analytics for early triage offers:
- End-to-end workflow optimization
- Appropriate routing of claims to straight-through processing or experienced or specialized adjusters, based on the complexity of the claim
- Increased consistency and streamlined workflows
- Enhanced communication and experience for customers
- Improved cost management
- Objective talking points for attorney-represented claims to improve adjustment accuracy
- Increased chance of identifying inflated or exaggerated claims
Benefits of Using Predictive Analytics to Improve Intelligent Decisioning & Adjuster Guidance
Utilizing predictive analytics can also help spur better decision-making and create more guidance opportunities with the claims process for adjusters. To give an example of how predictive analytics can facilitate smart decisioning and guide adjusters, let’s start by acknowledging that properly training new staff can be challenging; especially when the staff member’s average tenure is between 3.9 and 4.3 years (men and women, respectively), according to the U.S. Bureau of Labor Statistics in 2020. As many companies begin to eliminate the manual burden of paper-intensive processes and seek ways to incorporate more automation into their workflows, hundred-page three-ring training binders may cease to exist. Instead, claims organizations should focus on providing guidance to claims staff when they need it, through predictive analytics.
For more insight into how this type of adjuster guidance is applied, here is an example from the redesigned Mitchell Claims Examiner Portal, released earlier this year. On the medical bill detail screen, there is a section referred to as "Findings,” where alerts are surfaced that pinpoint conditions on the claim that an adjuster should pay close attention to. This includes updates such as “gap in treatment,” “delay in treatment” or “treatment extending past expected recovery date.” These are conditions that might be difficult for a claims examiner to spot and especially difficult to facilitate across an entire organization in a standardized way. But with intelligent decisioning and adjuster guidance, technology can guide the adjuster to conditions that are important to identify on the claim.
Here is a recap of the benefits that using predictive analytics for adjuster guidance provides:
- Reduces the need for manual processes and workflows
- Guides claims staff on key alerts and critical conditions
- Assists in the decision-making process
- Categorizes claims based on severity
Looking Ahead
As technology becomes increasingly prevalent in almost every aspect of today’s world, it’s not surprising that the workers’ compensation industry continues to rapidly evolve. While different technologies impact each claims organization uniquely, predictive analytics is paving the way to the forefront of smart technology as a whole. To read more about predictive analytics and how it is shaping the workers’ comp space, download our full 2021 trends report now.


